> At a Glance
> – Aetna initially refused to pay for Gabrielle Guerrero’s replacement partial-foot prosthesis, calling it “comfort” only
> – Guerrero’s mother charged $7,500 on a credit card so her daughter could walk at college graduation
> – Aetna reversed the denial after News Of Los Angeles asked questions, citing new clinical details
> – Why it matters: Insurers routinely reject prosthetics as “not medically necessary,” forcing patients into debt or lengthy appeals
A Texas woman who lost half her foot in a teenage off-road crash had to fight a six-month insurance battle to get a new walking prosthesis, spotlighting a pattern of denials that leaves thousands of amputees paying out-of-pocket or doing without.
Crash at 15, Denial at 21
Gabrielle Guerrero was 15 when an off-road vehicle hydro-planed and flipped, trapping her left foot. After two surgeries doctors partially amputated the foot, removing all toes and the front half.
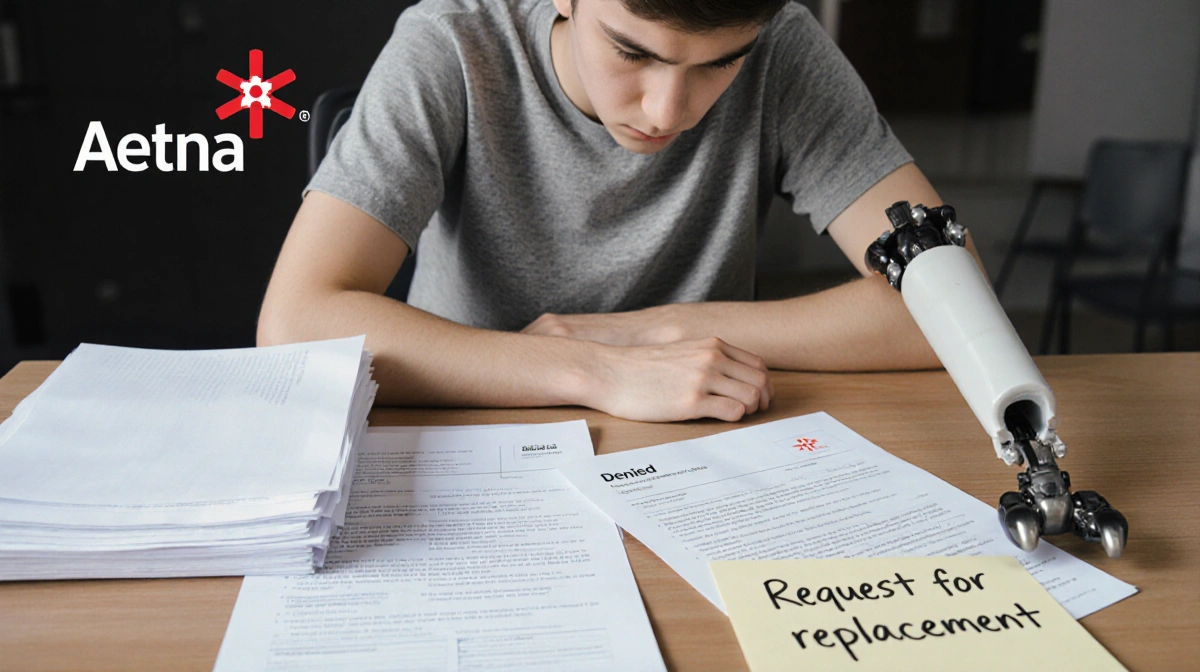
Now 21, she relies on a custom carbon-fiber prosthesis to walk without pain. “When I walk barefoot on hard floors, it’s very, very painful,” she said. “The prosthetic takes that pressure off.”
By 2024 the device was “literally disintegrating”: two fake toenails had fallen off and a rear split kept it from staying in place.
First Approval, Second Refusal
Her original prosthesis was fully covered by Aetna. When her prosthetist submitted the identical replacement request, the insurer denied it in September, stating:
- The claim was “improperly coded”
- A device “for appearance, comfort, or convenience is not considered medically necessary”
Guerrero appealed; a second denial arrived days before her December college graduation.
Racing the Clock
With commencement approaching, Guerrero’s mother paid the $7,500 balance on a credit card so the finished socket could be released.
> “It’s like a slap in the face,” Guerrero said. “My mom pays thousands in premiums and deductibles.”
| Timeline | Action |
|---|---|
| September | Aetna denies coverage |
| Early December | Olivia M. Hartwell contacts Aetna |
| Mid-December | Guerrero graduates, still unreimbursed |
| Day after graduation | Aetna cites missing clinical detail, upholds denial |
| One week later | Aetna reverses after receiving “critical information” |
Industry-Wide Pattern
Advocates say such denials are routine.
> “It’s not a matter of if you’ll be denied, but when,” said Nicole Ver Kuilen, director of impact campaigns for the Amputee Coalition.
Gerald Stark, president of the American Academy of Orthotists and Prosthetists, estimates “almost all” of his patients receive some form of refusal:
- Not medically necessary
- Not established care
- Out-of-network provider
Aetna’s Reversal
After News Of Los Angeles inquired, Aetna said the prosthetist “was unable to answer fundamental questions” during a peer-to-peer review and the requested device lacked proof it would “restore function and mobility.”
Days later the company rescinded the denial, telling News Of Los Angeles: “Now that we have more critical information… the plan sponsor has agreed to grant coverage.”
Guerrero’s mother was fully reimbursed.
Key Takeaways
- At least 25 states require state-regulated plans to match Medicare prosthetic coverage
- Multiple visits-Guerrero needed six-are common for proper fit
- Patients often travel 100 miles for qualified prosthetists
- Appeals succeed when additional clinical data is supplied
Guerrero, now walking pain-free in her new device, advised others: “Never give up… eventually they’ll say yes.”




